Sleep Apnea in Los Angeles, CA

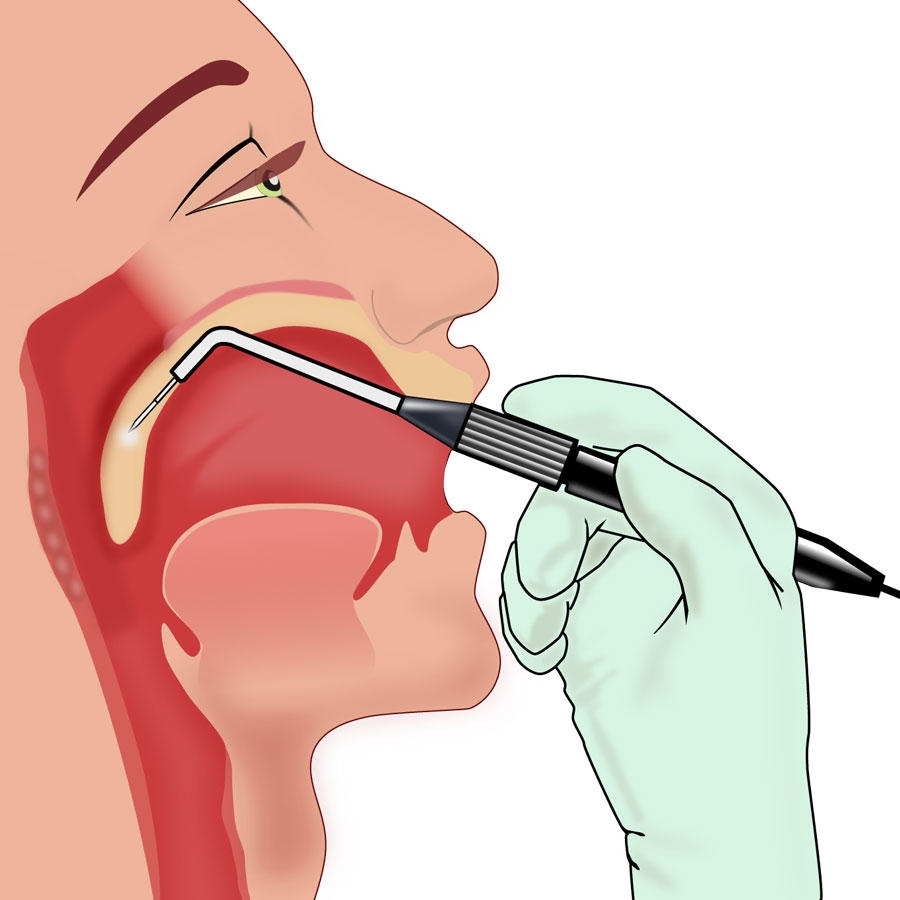
Sleep apnea, also spelled sleep apnoea, is a sleep disorder characterized by pauses in breathing or periods of shallow breathing during sleep. Each pause can last for a few seconds to a few minutes and they happen many times a night. In the most common form, this follows loud snoring. There may be a choking or snorting sound as breathing resumes. As it disrupts normal sleep, those affected may experience sleepiness or feel tired during the day. In children, it may cause problems in school or hyperactivity.
There are very effective tests for obstructive sleep apnea. Sinus Center Los Angeles has a board certified ENT that can order a medical grade sleep test in the comfort of your own home. He can also Rx a polysomnogram if central apnea of severe OSA is suspected.
There are three forms of sleep apnea: obstructive (OSA), central (CSA), and a combination of the two called mixed.
OSA is the most common form. Risk factors for OSA include being overweight, a family history of the condition, allergies, a small airway, and enlarged tonsils. In OSA, breathing is interrupted by a blockage of airflow, while in CSA breathing stops due to a lack of effort to breathe.
People with sleep apnea may not be aware they have it. In many cases, it is first observed by a family member. Sleep apnea is often diagnosed with a medical grade at home or overnight sleep study.
Treatment may include lifestyle changes, custom made mandibular posturing devices made in our onsite state of the art laboratory.
Other modalities include breathing devices.
Jaw surgery may also be recommended.
Lifestyle changes may include avoiding alcohol, losing weight, stopping smoking, and sleeping on one’s side.
Breathing devices include the use of a CPAP machine.
Do you feel tired in the mornings when you awaken? Some people may feel despondent, depressed, or suffer despair and anxiety. Others may suspect cognitive impairment, memory loss and tiredness at the end of the day.
Without treatment sleep apnea may increase the risk of heart attack, stroke, diabetes, heart failure, irregular heartbeat, obesity, motor vehicle collisions and if progressive and severe can cause death.
Sleep disorders, including sleep apnea, have become a significant health issue in the United States. The American Academy of Sleep Medicine estimates that more than 22 million Americans suffer from sleep apnea. More than 18 million Americans have moderate or severe obstructive and are suffering unnecessarily including with progressive health deterioration, despondency, depression, memory loss, cognitive impairment, diabetes, and heart disease.
Unfortunately, most of these people are not aware they have sleep apnea. OSA, when left untreated, can lead to high blood pressure, chronic heart failure, atrial fibrillation, stroke, and other cardiovascular problems and is a factor in many traffic accidents and accidents with heavy machinery, owing to the persistent drowsiness suffered by many OSA patients before the disease is recognized and treated.
Fortunately, specialists at Jaw Surgery Los Angeles and Sinus Center Los Angeles and OrthodonticCenter.LA have tests to diagnose obstructive sleep apnea as well as very effective treatment modalities.
Signs and Symptoms
People with sleep apnea have problems with excessive daytime sleepiness (EDS), impaired alertness, and vision problems. OSA may increase risk for driving accidents and work-related accidents. If OSA is not treated, people are at increased risk of other health problems, such as diabetes. Death could occur from untreated OSA due to lack of oxygen to the body. Moreover, people are examined using “standard test batteries” to further identify parts of the brain that may be adversely affected by sleep apnea, including those that govern:
- “executive functioning”, the way the person plans and initiates tasks
- paying attention, working effectively and processing information when in a waking state
- using memory and learning.
Do you:
1.Awaken in the morning feeling tired and not fully rejuvenated?
Many people think that they are tired in the morning due to work, stress, poor exercise, poor diet, or age. However, it may be simply due to mild or moderate of severe obstructive sleep apnea. Fortunately there are very effective treatments available and it is possible to wake up each morning feeling fully rejuvenated and ready for a productive day.
2.Snore while sleeping?
Did you know that snoring in children and adults is NOT normal and can adversely affect your health by not allowing sufficient oxygen to your brain while sleeping.
Fortunately, very effective treatments are available.
Sleep apnea can affect people regardless of sex, race, or age. However, risk factors include:
- Being male
- Excessive weight
- An age above 40
- Large neck size (greater than 16–17 inches)
- Enlarged tonsils or tongue
- Small or recessed jaw
- Gastroesophageal reflux
- Allergies
- Sinus problems
- A family history of sleep apnea
- Deviated septum
Alcohol, sedatives and tranquilizers may also promote sleep apnea by relaxing throat muscles. Smokers have sleep apnea at three times the rate of people who have never smoked.
Central sleep apnea is more often associated with any of the following risk factors:
- Being male
- An age above 65
- Having heart disorders such as atrial fibrillation or atrial septal defects such as PFO
- Stroke
High blood pressure and diabetes is very common in people with sleep apnea.
Surgery
There are very effective procedures (sleep surgery) to treat sleep apnea. These include surgical and non-surgical options. Specialists at Jaw Surgery Los Angeles and Sinus Center Los Angeles (www.sinuscenter.la) are trained in sleep medicine and plan the jaw surgery to optimize the jaw, face and airway anatomy for best function, esthetics, and best breathing including oxygen uptake, especially while sleeping. The airway includes the entire airway and the area behind the tongue (retro-glosssal area) and inside the nose.
NASAL OBSTRUCTION
Specialists at Sinus Center Los Angeles have proprietary 3-D digital imaging to help visualize the nasal anatomy and evaluate for any blockage. Effective treatments include non-surgical and surgical treatments with minimal ‘downtime’ and recovery. They collaborate with specialists at Jaw Surgery Los Angeles to co-ordinate procedures as independent treatments or in conjunction with your jaw surgery.
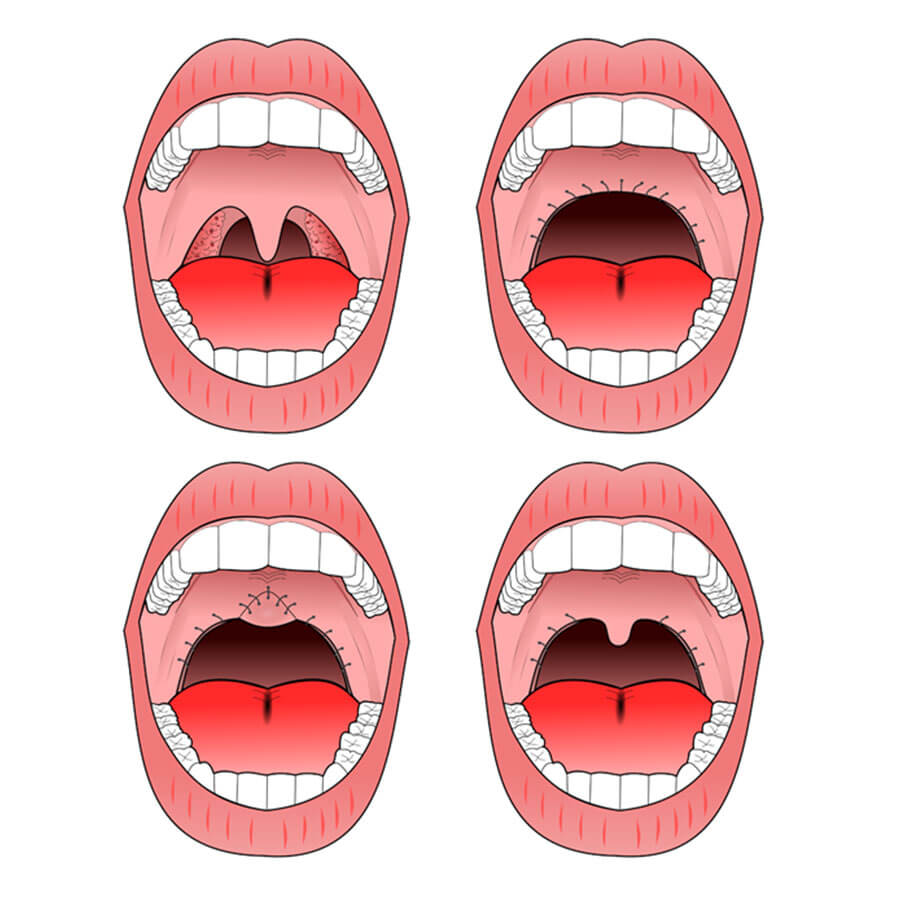
Image Credit
Uvulopalatopharyngoplasty. A) pre-operative, B) original UPPP, C) modified UPPP, and D) minimal UPPP.
PHARYNGEAL OBSTRUCTION
Tonsillectomy and uvulopalatopharyngoplasty (UPPP or UP3) are available to address pharyngeal obstruction.
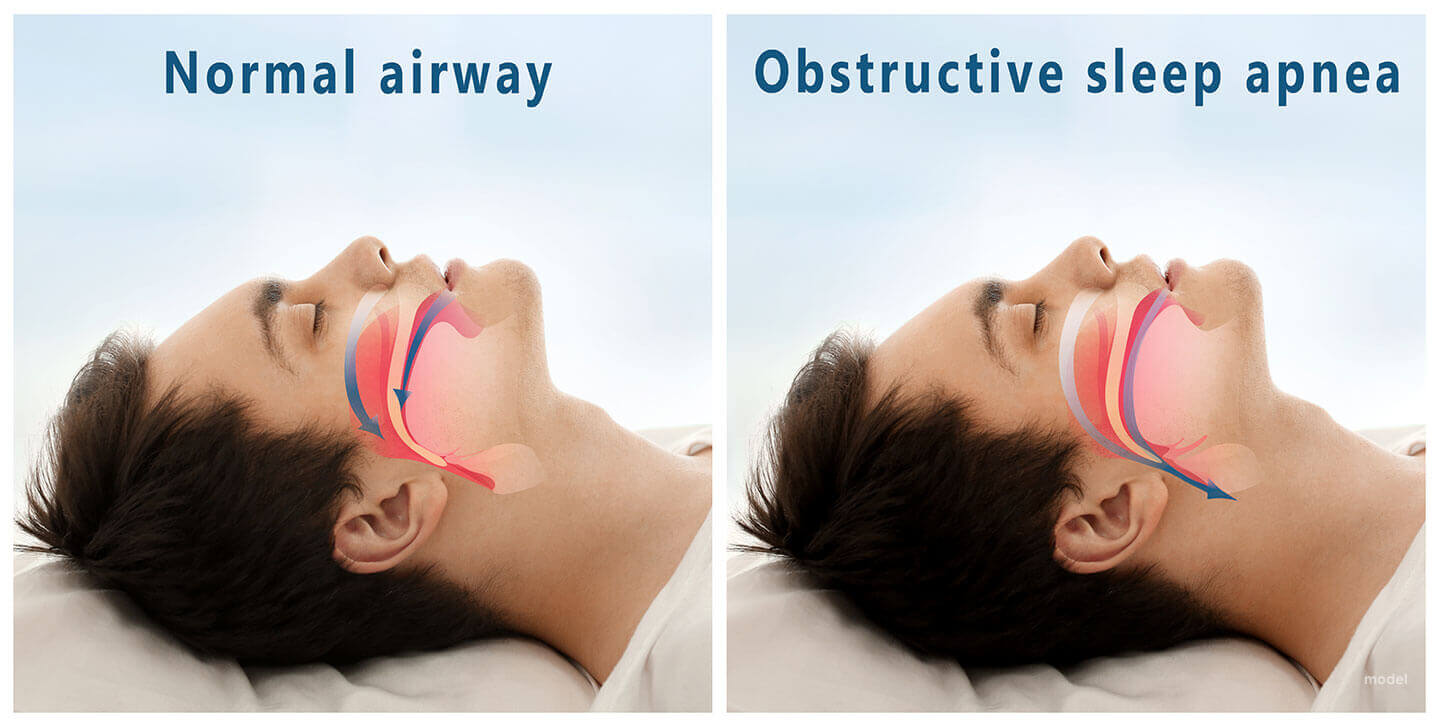
The “Pillar” device is one treatment for snoring and obstructive sleep apnea. This consists of thin, narrow strips of polyester that are inserted into the roof of the mouth (the soft palate) using a modified syringe and local anesthetic, in order to stiffen the soft palate. This procedure addresses one of the most common causes of snoring and sleep apnea — vibration or collapse of the soft palate. It was approved by the FDA for snoring in 2002 and for obstructive sleep apnea in 2004. A 2013 meta-analysis found that “the Pillar implant has a moderate effect on snoring and mild-to-moderate obstructive sleep apnea” and that more studies with a higher level of evidence were needed to arrive at a definite conclusion. Complications include the polyester strips working their way out of the soft palate in about 10% of the people in whom they are implanted.
Fortunately are are numerous other more effective treatment options
HYPOPHARYNGEAL OR BASE OF TONGUE OBSTRUCTION
Base-of-tongue advancement by means of advancing the chin and genial tubercles of the mandible are performed in an out patient setting in our AAAHC OR.
Tongue suspension, or hyoid suspension (aka hyoid myotomy and suspension or hyoid advancement) can also help with the lower pharynx airway obstruction.
Other surgery options include shrinking or stiffening the excess tissue at the back of the mouth or throat, or removing the excess tissue using a procedure called a partial uvulectomy. This procedure can be done in the office using a local anesthesia or in our AAAHC OR under light sedation.
(Please see www.SinusCenter.LA
Jaw Surgery is very effective for OSA
The Stanford Center for Excellence in Sleep Disorders Medicine achieved a 95% cure rate in people with obstructive sleep apnea with Orthognathic Surgery.
Maxillo-mandibular advancement (MMA) is considered the most effective surgery for people with obstructive sleep apnea, because it increases the posterior airway space (PAS).
The main benefit of the operation is that the oxygen saturation in the arterial blood increases, with a normal airway.
In a study published in 2008, 93.3.% of surgery patients achieved a significant improvement of their quality of life, based on the Functional Outcomes of Sleep Questionnaire (FOSQ). Surgery led to a significant increase in overall health, general productivity, social outcome, activity level, vigilance, intimacy, and intercourse.
Overall risks of MMA surgery are low: The Stanford University Sleep Disorders Center found 4 failures in a series of 177 patients, or about one out of 44 patients. Health professionals are often untrained as to who should be referred for surgery and when to do so.
Indications for surgery include failed use of CPAP or mandibular posturing device use, skeletal imbalance and malocclusions (bad bites).
Maxillo-mandibular advancement surgery is often combined with a genioglossal advancement, for obstructive sleep apnea.
POTENTIAL COMPLICATIONS
Complications will be discussed in detail for your specific condition. You will also be given written informed consent forms describing the risks, options, alternative and limitations. Below are a few general potential complications.
Several inpatient and outpatient procedures use sedation. Many drugs and agents used during surgery to relieve pain and to depress consciousness remain in the body at low amounts for hours or even days afterwards. In an individual with either central, obstructive or mixed sleep apnea, these low doses may be enough to cause life-threatening irregularities in breathing or collapses in a patient’s airways. Use of analgesics and sedatives in these patients postoperatively should therefore be minimized or avoided.
Surgery on the mouth and throat, as well as dental surgery and procedures, can result in postoperative swelling of the lining of the mouth and other areas that affect the airway. Even when the surgical procedure is designed to improve the airway, such as tonsillectomy and adenoidectomy or tongue reduction, swelling may negate some of the effects in the immediate postoperative period. Once the swelling resolves and the palate becomes tightened by postoperative scarring, however, the full benefit of the surgery may be appreciated.
A person with sleep apnea undergoing any medical treatment must make sure his or her doctor and anesthetist are informed about the sleep apnea. Alternative and emergency procedures may be necessary to maintain the airway of patients with sleep apnea.